
As Ray Anthony has sought gender affirming care over the years, they often found access was “a dice game.” They said it was only through their knowledge of the medical system — and of their rights — that they persisted.
Now Anthony, who identifies as trans, uses that knowledge to help others in their role as Planned Parenthood Columbia Willamette’s first gender affirming care patient navigator.
“If somebody is on the phone with me, and they’re crying because they can’t access their medication, I can be like, ‘I know, this is important,’” Anthony said. “And I actually know it’s important.”
In an interview with The Lund Report, Anthony reflected on their first year in the new position and the challenges that gender-diverse patients face.
And how it’s been a job in which Anthony has been increasingly busy.
Like other local providers of gender affirming care, Planned Parenthood has seen a recent surge in demand for services as gender diverse patients flee Republican-controlled states that have enacted anti-transgender legislation. The migration has put expertise like Anthony’s in high demand.
In 2021, Planned Parenthood Columbia Willamette provided gender affirming care to about 800 individuals. Planned Parenthood offers hormone care for people who are transitioning but does not perform surgical procedures. In 2022, its gender affirming care clientele jumped 25% to more than 1,000, and already this year more than 1,300 individuals have received such services.
“As we’re watching more and more hideous bans come into play, and services being denied, and services actually not even available, I think the bigger picture is that (demand) is only going to continue to grow as we see the need grow,” said Kristi Scdoris, spokesperson for the local Planned Parenthood affiliate, which operates clinics in Oregon and southwest Washington.
Anthony spends their days jumping from call to call, advising callers on everything from name changes to housing resources and providing surgical referrals. But most often they are weaving together resources and making connections to help people access what can be stigmatizing services and medications that pharmacists aren’t always eager to provide.
Anthony, 36, said their job is a perfect match for the way their brain works: “like a spider web.”
Connect with a navigator
Several local health care providers recognize Oregon’s role as an access point to transgender health care and have hired patient navigators to assist patients seeking gender affirming care. Connect with a navigator through the following links:
Planned Parenthood Columbia Willamette
Oregon Health & Science University
Legacy Health
Even in a state that’s perceived as welcoming of gender diverse patients, navigating the system of care and finding the right providers is a complex journey that can often result in awkward interactions and barriers to treatment, Anthony said.
“I’ve had pharmacies that fully have been transphobic,” Anthony said. They said some pharmacists won’t use a patient’s preferred name or otherwise treat them poorly when they’re trying to fill a prescription for hormone therapy — and that can happen anywhere in the state. “It doesn’t have to be rural Oregon,” Anthony said. “Bias is everywhere.”
Anthony points callers to trans-friendly pharmacies and offers medications by mail. They also help people who aren’t Planned Parenthood patients avoid awkward phone calls by calling around to clinics in rural areas to see where gender affirming care can be accessed. “It’s very hard to vet,” they said, adding that patients get discouraged after calling a clinic and getting a negative response.
Anthony also fields frequent out of state calls — especially from Florida — offering advice to people who are planning to move to Oregon. One of the biggest needs is getting around patient waitlists. Anthony said callers don’t want to delay treatment for months upon their arrival because they can’t get insurance coverage or must wait weeks for an office visit.
Nearly 500 anti-trans bills have been introduced across the U.S. this year, according to the American Civil Liberties Union. Four were passed into law in Florida. Seven were also introduced in Oregon, but they failed to advance. Instead, Oregon lawmakers doubled down on protections and passed House Bill 2002, which expanded the range of gender affirming care procedures that insurance companies must cover.
“I don’t think people really know how important access to care is — that is quality and informed care — for trans, non-binary and gender diverse populations,” Anthony said. “But we’re changing that.”
Barriers to coverage
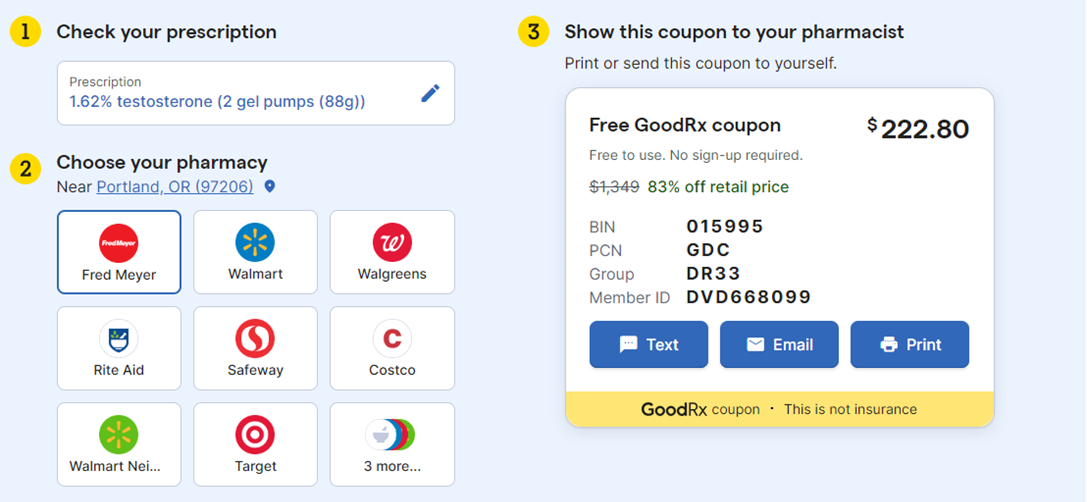
Anthony estimates that about 30% of their patients receive gender affirming care that isn’t covered by insurance, forcing them to pay out of pocket. Hormone therapies alone can retail from about $47 to $1,300 per month, according to prices listed on GoodRx. Sometimes coupons are available, but patients don’t always know that.
House Bill 2002
H.B. 2002 goes into effect Jan. 1, 2024. The abortion and gender affirming care bill — which became the focal point of Senate Republicans’ walkout in the last legislative session — will expand the range of procedures that insurance companies are required to cover, such as the costly hair removal required before some gender reassignment surgeries.
It will not, however, change criteria a patient must meet to access care.
According to the Oregon Department of Consumer and Business Services, H.B. 2002 will prohibit insurance companies from offering a health benefit plan in Oregon that:
denies or limits coverage for gender-affirming treatment that is medically necessary as determined by the prescribing provider
applies categorical cosmetic or blanket exclusions to medically necessary gender-affirming treatment
excludes medically necessary gender-affirming procedures, such as tracheal shaves, hair electrolysis and facial feminization surgery, as cosmetic services
denies or limits access to gender-affirming treatment unless a health care provider with experience in gender-affirming treatment has first reviewed and approved the denial or limitation
It also:
requires a health benefit plan to include a sufficient number of gender-affirming treatment providers in their networks to ensure geographic access
applies to comprehensive health insurance plans, including those sold on the Oregon Health Insurance Marketplace and group plans sold to Oregon employers that are issued or renewed on or after Jan. 1, 2024
applies to coverage provided under the Oregon Health Plan
explicitly prohibits insurers from excluding coverage of medically necessary gender-affirming care services on the basis that the services are “cosmetic” in nature
Planned Parenthood Columbia Willamette spokesperson Scdoris noted that to receive gender-affirming health care at all, a patient must meet the following requirements:
- Persistent well-documented gender dysphoria (a condition of feeling one’s emotional and psychological identity as male or female to be opposite to one’s biological sex) diagnosed by a mental health professional well-versed in the field
- Capacity to make a fully informed decision and to consent to treatment
- Age 15 or older
- Good control of significant medical and/or mental comorbid conditions
“Having to prove they are transgender, genderfluid, nonbinary, etc. is difficult for patients — especially as Oregon and the United States experience a mental health care access shortage,” Scdoris told The Lund Report in an email.
Anthony noted that acquiring a letter from a mental health professional means crossing over from physical care to mental health care, which carries an additional layer of stigma and barriers to access.
Anthony said that sometimes they discover when calling a patient’s insurer that their employer has opted for a plan that doesn’t cover “that type of care.” This is likely a reference to benefit categories, not specifically gender affirming care. That’s because, in Oregon, health benefit plans are required to cover medically necessary hormone treatment for gender-affirming care if the plan would cover the same treatment provided for other purposes, according to state rules that were enacted in 2016.
One of the most frequent barriers is obtaining prior authorization from an insurer for prescription benefits, said Anthony. “Depending on their guidelines, if you don’t hit certain criteria, then certain medications aren’t approved,” they said.
Scdoris noted that Planned Parenthood sees some patients denied access to gender affirming medication because they have a common co-occurring diagnosis, such as depression.
“There’s is so much criteria for folks to be themselves and get medications that make them feel aligned that is just baffling to me,” Anthony said.
When prior authorization is denied, Anthony tells patients to appeal.
Patients in Oregon have 180 days from the date they are notified of a denial to appeal. Health plan providers can instruct patients on how to appeal their claim.
If the appeal is denied, Anthony tells patients to report it to the Oregon Department of Business and Consumer Services.
According to Mark Peterson, a spokesperson for the agency, the department has received 10 complaints related to denied gender affirming care since the start of last year. Four of those complaints were against plans that were offered by self-insured employers, which are exempt from state regulations.
“Therefore, some health plans in Oregon may continue to deny coverage for these services despite state laws requiring coverage,” Peterson said in an email.
He said patients may have the right to have their cases reviewed externally by a third party if their claim on appeal is denied.
